Rooted in a biomedical, institutional model of care, reactive to short-term reimbursement and real estate incentives and often hampered by siloed local planning efforts, America’s institutional long-term care, aging and disability service sectors have failed to provide communities with what we all want and need as we grow older and seek to remain integrated with multi-ability, multi-generational, inclusive community life. Despite landmark laws, including the Nursing Home Reform Act of 1987 and the Americans with Disabilities Act of 1990, many service silos remain stubbornly in place.
Yet when we step back and look at the array of community partners and providers who are expert in housing and providing skilled care, moderate level care and light-touch care and supports that improve quality of life, it becomes clear we can change this -- by building a new Connected Community model to make the old modes obsolete.
We are inviting community leaders around the US to step forward to help create high-performance systems of supportive care that are embedded in normal community life. To start, we’re looking to recruit 100 Connected Communities over the next 3 years with the help of top talent in the movement of person-directed living. Evidence-based solutions exist today in pockets of the housing and skilled care sectors, developed over decades of work by leaders who have long experience in designing and implementing cost-effective change -- innovators involved with the Center for Innovation’s Green House Project and Pioneer Network (together now known as AgingIN), the Eden Alternative, the Live Oak Project, the Gray Panthers and other innovators with a focus on community living, including PACE (Program of All-Inclusive Care for the Elderly), Area Agencies on Aging, Caring Across Generations, Age-Friendly Communities, and many more.
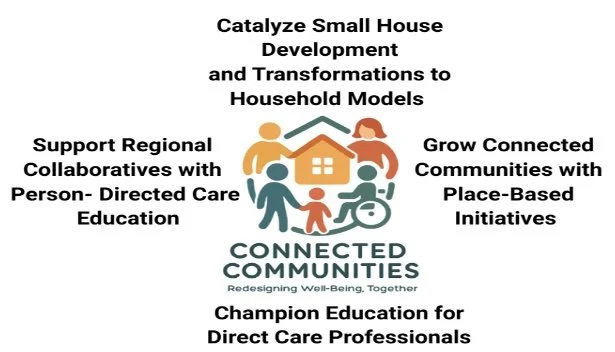
Creating Connected Communities that offer a vibrant Long-Term Services and Supports (LTSS) continuum of care for our long-lived society involves four building blocks. These elements comprise an actionable overall framing and an organized working plan.
The first is comprehensive person-directed living education for leadership and all team members, including Direct Care Professionals (DCP), who are working for organizations across the aging and disability spectrum in a defined geography.
Core elements of culture change education are being synthesized from existing training and organizational development resources, including The Eden Alternative’s “Principles and Domains of Well Being,” Action Pact’s “In Pursuit of the Sunbeam” and “Tales of Transformation” UNC’s “Bathing Without a Battle,” training in empowerment, conflict resolution, mindfulness, communication and the use of learning circles and community meetings and discussions of the definition of an elder.
Areas of sustainability are also being defined, including how to identify a staffer to lead as an internal Culture Champion; use of continuing education to sustain person-centered care practices; ways to encourage personal engagement and wider community engagement
A key focus will be on positive accountability, financial transparency, and syncing training and practices with evolving value-based payment models and licensure and certification standards.
Shared education and person-centered practices across organizations will be strengthened with outcomes tracking that includes resident experience of care and quality of life metrics, dementia care metrics, leadership metrics, and interdisciplinary team internal assessments of progress as well as barriers in shifting to person-directed care, together with assessment of financial impact. Existing tools such as the “Artifacts of Culture Change 2.0” can track these outcomes across settings and services, where appropriate.
The second element aims to inspire state and local planning processes to take a role in supporting and developing new small home models and adaptation of traditional nursing homes to become small house or household model configurations, which feature:
Private bedrooms and bathrooms available for all who want them
Autonomous household units of 1-18 residents (depending on cost analyses and community preference)
Defined kitchens that prep and serve food
Safe access to the outdoors and community life for all
Adoption of organizational structure/behaviors and leadership philosophies/ practices conducive to resident-directed living
Regular processes holding care professionals, administration, and other team members accountable to resident-defined measures of quality of life and care
Decision-making bodies and processes inclusive of and accountable to residents and their representatives or loved ones
Regular, evidence-based training in culture change/resident-directed living for all care partners, providers, and other team members
The third element concentrates on empowerment and expansion of Direct Care Professionals through creation of:
Free online educational videos and trainings, grounded in person-directed LTSS core competencies and designed to be ultimately incorporated into current state and federal education standards across all LTSS settings and populations. The videos and trainings would incentivize states and employers to consider dropping portability barriers, facilitate recruitment across the LTSS sector, and improve the recognition of person-centered DCP training.
In-person skills demonstrations and designed to be suitable for a wide range of positions, including residential, community-based, and in-home settings.
Educational modules accompanied by a national Care Force Marketing Campaign tailored to reach individuals from a wide variety of backgrounds and ages in an organized mass recruiting initiative linked to organizations and culture change competencies developed collaboratively.
The last element is the logical culmination of work done to advance the other elements to design and stand-up Connected Communities. Making this happen involves place-based collaborative work to engage community economic development organizations, local political leaders, housing experts and lending institutions, and other stakeholders collaborating with an array of LTSS providers to embed a continuum-of-care delivery system in their geographic communities.
Contact Information: Anne Montgomery, anneheathmontgomery@gmail.com 202.492.9299
Joe Angelelli, joeangelelli@gmail.com 412-304-1463